End Stage Renal Disease (ESRD)
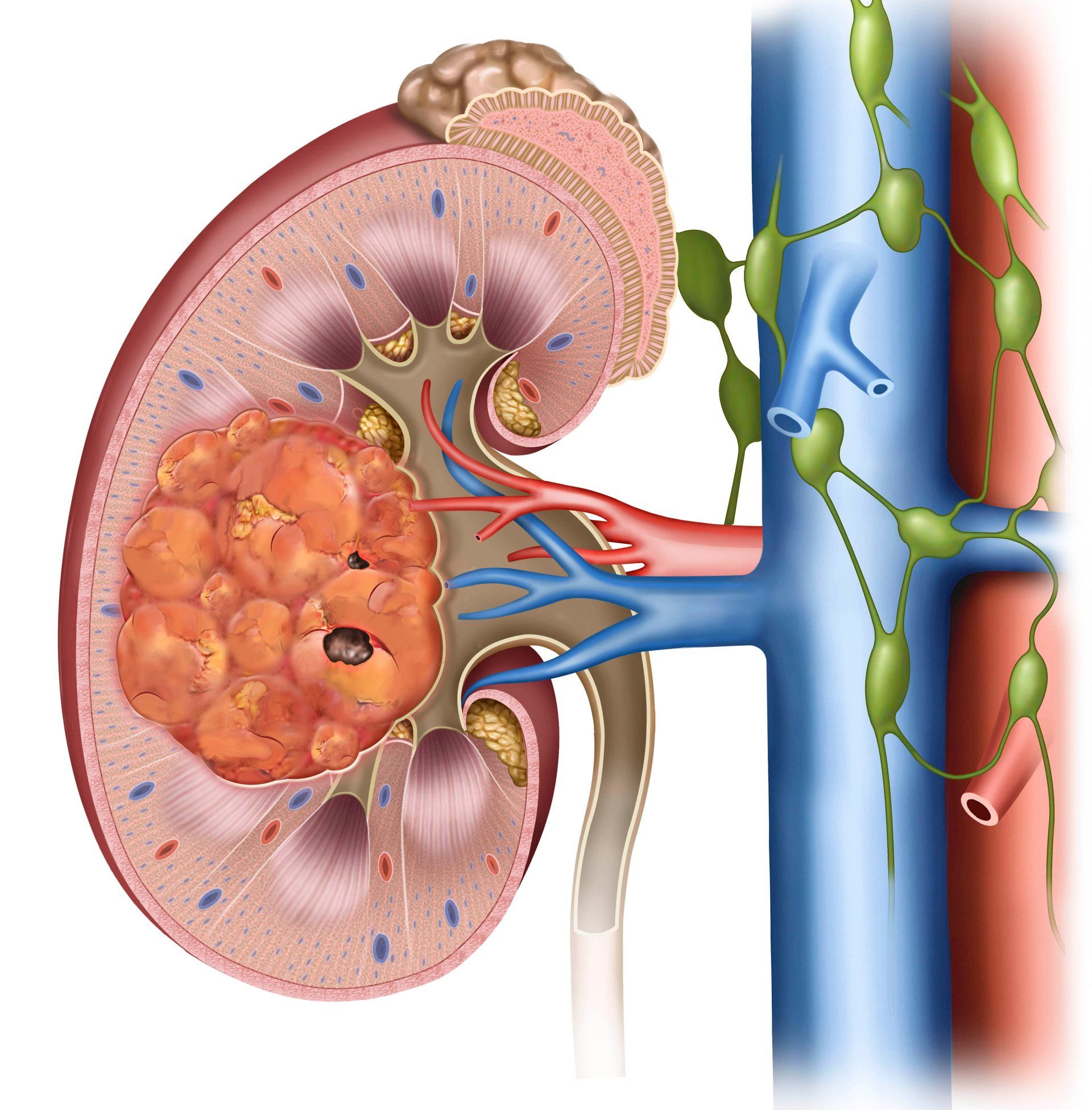
Acute renal failure is when your kidneys suddenly fail for some reason and fail to clean and filter your blood. This is an emergency.
Renal insufficiency is a problem with the kidneys filtering toxins from the blood appropriately. It can be treated medically by your primary care provider. If it worsens, or you develop acute renal failure, you may be referred to a kidney specialist (nephrologist).
Kidney insufficiency and kidney failure most often occur in patients with diabetes and poorly controlled high blood pressure (hypertension). Other risk factors include some medications, severe dehydration, contrast (dye given for CT scans, heart cath, and arteriograms/venograms), drug abuse, and other rare conditions.
End stage renal disease is when your kidneys have failed completely and most often will not recover. Until you have a kidney transplant, you will need dialysis treatments to clean and filter your blood. Of course, kidney transplant is a very specialized procedure performed in academic institutions in big cities like Nashville or St. Louis. Unfortunately, there are not enough kidneys to give everyone a transplant. Some patients may not be a candidate for a kidney transplant because of age or comorbid conditions like advanced heart and lung disease.
Peritoneal dialysis occurs through a catheter/tube in your abdominal cavity. Many people dialyze this way, but it requires a lot of training as it's performed at home. If you and your nephrologist decide that peritoneal dialysis is your best option, you will be referred to a general surgeon who will place your peritoneal dialysis catheter in the operating room.
Most people with end stage renal disease (ESRD) are treated with hemodialysis at a dialysis center (or at home by some patients). In this case, you will be referred to Paducah Vascular Institute for a hemodialysis access procedure. Hemodialysis is when your blood is filtered by a machine.
Hemodialysis Access Procedures
Hemodialysis catheter
This is a large intravenous line placed in the groin or neck veins (most commonly the internal jugular vein). This tip of the line is in the vena cava. The other end sticking out of your skin has two sides. The dialysis machine sucks blood out of one side and filters it through the machine. The machine then pushes the blood back into your body through the other side so the blood is constantly circulating. This is not a good long term solution because of the risks of blood infection and the vena cava or jugular vein closing off.
Arteriovenous fistula (AV Fistula)
A connection made by the vascular surgeon in the operating room between an artery and vein allowing the vein to become larger and carry a lot of blood. It takes at least 6 weeks for the vein to mature (get big enough and strong enough to use for hemodialysis). The dialysis nurses put two needles through the skin into the vein and hook those needles up to the dialysis machine to circulate the blood through the machine while filtering the blood. Typically, hemodialysis treatments are three times per week.
Arteriovenous graft (AV graft)
When a patient doesn't have good veins t ocreate a fistula, an AV graft can be used. An AV graft is created by a vascular surgeon in the operating room. An artificial piece of tubing (graft) is tunneled underneath the skin. One side of this graft is tied into the artery and the other side tied into the vein. This tube is then punctured in two places like a fistula for dialysis treatments three times per week.
Fistulogram or AV graft angiogram
When your av fistula or graft isn't working well, the nephrologist may send you to a vascular surgeon for a fistulogram or an AV graft angiogram. This is an Xray study of the fistula or graft to detect any narrowing or blockages in the artery, vein, or graft. It can be performed most often in the office with local anesthesia and intravenous/moderate sedation. If there is any narrowing it can be treated with balloons and/or stents. If the fistula or graft is clotted, it may require clot busting medicine to dissolve the clot followed by balloons and/or stents.